Psychology Behind Problem Gambling
A meta-analysis of surveys of problem gambling prevalence in Australia and New Zealand with respect to concentration of electronic gaming machines. International Gambling Studies, 9(3), 225-244. Doi: 10.10; Blaszczynski, A., & Nower, L. A pathways model of problem and pathological gambling. Addiction,97, 487-499. Gambling addiction can occur when a person feels that they are in financial ruin and can only solve their problems by gambling what little they have in an attempt to get a large sum of money. Unfortunately, this almost always leads to a cycle in which the gambler feels they must win back their losses, and the cycle goes on until the person is.
When Shirley was in her mid-20s she and some friends road-tripped to Las Vegas on a lark. That was the first time she gambled. Around a decade later, while working as an attorney on the East Coast, she would occasionally sojourn in Atlantic City. By her late 40s, however, she was skipping work four times a week to visit newly opened casinos in Connecticut. She played blackjack almost exclusively, often risking thousands of dollars each round—then scrounging under her car seat for 35 cents to pay the toll on the way home. Ultimately, Shirley bet every dime she earned and maxed out multiple credit cards. “I wanted to gamble all the time,” she says. “I loved it—I loved that high I felt.”
In 2001 the law intervened. Shirley was convicted of stealing a great deal of money from her clients and spent two years in prison. Along the way she started attending Gamblers Anonymous meetings, seeing a therapist and remaking her life. “I realized I had become addicted,” she says. “It took me a long time to say I was an addict, but I was, just like any other.”
Ten years ago the idea that someone could become addicted to a habit like gambling the way a person gets hooked on a drug was controversial. Back then, Shirley's counselors never told her she was an addict; she decided that for herself. Now researchers agree that in some cases gambling is a true addiction.
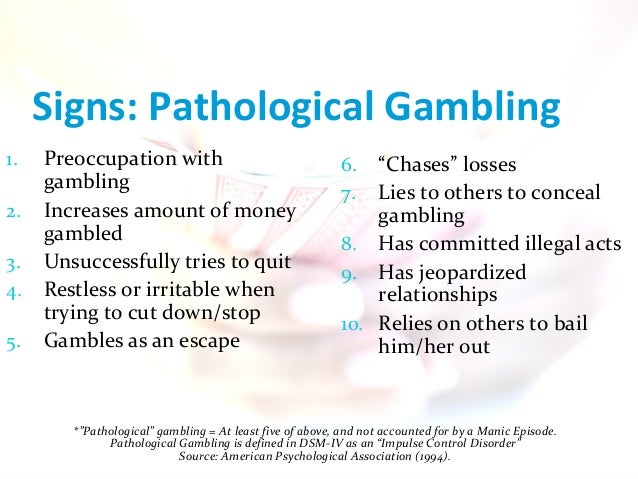
In the past, the psychiatric community generally regarded pathological gambling as more of a compulsion than an addiction—a behavior primarily motivated by the need to relieve anxiety rather than a craving for intense pleasure. In the 1980s, while updating the Diagnostic and Statistical Manual of Mental Disorders (DSM), the American Psychiatric Association (APA) officially classified pathological gambling as an impulse-control disorder—a fuzzy label for a group of somewhat related illnesses that, at the time, included kleptomania, pyromania and trichotillomania (hairpulling). In what has come to be regarded as a landmark decision, the association moved pathological gambling to the addictions chapter in the manual's latest edition, the DSM-5, published this past May. The decision, which followed 15 years of deliberation, reflects a new understanding of the biology underlying addiction and has already changed the way psychiatrists help people who cannot stop gambling.
More effective treatment is increasingly necessary because gambling is more acceptable and accessible than ever before. Four in five Americans say they have gambled at least once in their lives. With the exception of Hawaii and Utah, every state in the country offers some form of legalized gambling. And today you do not even need to leave your house to gamble—all you need is an Internet connection or a phone. Various surveys have determined that around two million people in the U.S. are addicted to gambling, and for as many as 20 million citizens the habit seriously interferes with work and social life.
Two of a Kind
The APA based its decision on numerous recent studies in psychology, neuroscience and genetics demonstrating that gambling and drug addiction are far more similar than previously realized. Research in the past two decades has dramatically improved neuroscientists' working model of how the brain changes as an addiction develops. In the middle of our cranium, a series of circuits known as the reward system links various scattered brain regions involved in memory, movement, pleasure and motivation. When we engage in an activity that keeps us alive or helps us pass on our genes, neurons in the reward system squirt out a chemical messenger called dopamine, giving us a little wave of satisfaction and encouraging us to make a habit of enjoying hearty meals and romps in the sack. When stimulated by amphetamine, cocaine or other addictive drugs, the reward system disperses up to 10 times more dopamine than usual.
Continuous use of such drugs robs them of their power to induce euphoria. Addictive substances keep the brain so awash in dopamine that it eventually adapts by producing less of the molecule and becoming less responsive to its effects. As a consequence, addicts build up a tolerance to a drug, needing larger and larger amounts to get high. In severe addiction, people also go through withdrawal—they feel physically ill, cannot sleep and shake uncontrollably—if their brain is deprived of a dopamine-stimulating substance for too long. At the same time, neural pathways connecting the reward circuit to the prefrontal cortex weaken. Resting just above and behind the eyes, the prefrontal cortex helps people tame impulses. In other words, the more an addict uses a drug, the harder it becomes to stop.
Research to date shows that pathological gamblers and drug addicts share many of the same genetic predispositions for impulsivity and reward seeking. Just as substance addicts require increasingly strong hits to get high, compulsive gamblers pursue ever riskier ventures. Likewise, both drug addicts and problem gamblers endure symptoms of withdrawal when separated from the chemical or thrill they desire. And a few studies suggest that some people are especially vulnerable to both drug addiction and compulsive gambling because their reward circuitry is inherently underactive—which may partially explain why they seek big thrills in the first place.
Even more compelling, neuroscientists have learned that drugs and gambling alter many of the same brain circuits in similar ways. These insights come from studies of blood flow and electrical activity in people's brains as they complete various tasks on computers that either mimic casino games or test their impulse control. In some experiments, virtual cards selected from different decks earn or lose a player money; other tasks challenge someone to respond quickly to certain images that flash on a screen but not to react to others.
A 2005 German study using such a card game suggests problem gamblers—like drug addicts—have lost sensitivity to their high: when winning, subjects had lower than typical electrical activity in a key region of the brain's reward system. In a 2003 study at Yale University and a 2012 study at the University of Amsterdam, pathological gamblers taking tests that measured their impulsivity had unusually low levels of electrical activity in prefrontal brain regions that help people assess risks and suppress instincts. Drug addicts also often have a listless prefrontal cortex.
Psychology Behind Problem Gambling Definition
Further evidence that gambling and drugs change the brain in similar ways surfaced in an unexpected group of people: those with the neurodegenerative disorder Parkinson's disease. Characterized by muscle stiffness and tremors, Parkinson's is caused by the death of dopamine-producing neurons in a section of the midbrain. Over the decades researchers noticed that a remarkably high number of Parkinson's patients—between 2 and 7 percent—are compulsive gamblers. Treatment for one disorder most likely contributes to another. To ease symptoms of Parkinson's, some patients take levodopa and other drugs that increase dopamine levels. Researchers think that in some cases the resulting chemical influx modifies the brain in a way that makes risks and rewards—say, those in a game of poker—more appealing and rash decisions more difficult to resist.
A new understanding of compulsive gambling has also helped scientists redefine addiction itself. Whereas experts used to think of addiction as dependency on a chemical, they now define it as repeatedly pursuing a rewarding experience despite serious repercussions. That experience could be the high of cocaine or heroin or the thrill of doubling one's money at the casino. “The past idea was that you need to ingest a drug that changes neurochemistry in the brain to get addicted, but we now know that just about anything we do alters the brain,” says Timothy Fong, a psychiatrist and addiction expert at the University of California, Los Angeles. “It makes sense that some highly rewarding behaviors, like gambling, can cause dramatic [physical] changes, too.”
Gaming the System
Psychology Behind Problem Gambling Problem
Redefining compulsive gambling as an addiction is not mere semantics: therapists have already found that pathological gamblers respond much better to medication and therapy typically used for addictions rather than strategies for taming compulsions such as trichotillomania. For reasons that remain unclear, certain antidepressants alleviate the symptoms of some impulse-control disorders; they have never worked as well for pathological gambling, however. Medications used to treat substance addictions have proved much more effective. Opioid antagonists, such as naltrexone, indirectly inhibit brain cells from producing dopamine, thereby reducing cravings.
Dozens of studies confirm that another effective treatment for addiction is cognitive-behavior therapy, which teaches people to resist unwanted thoughts and habits. Gambling addicts may, for example, learn to confront irrational beliefs, namely the notion that a string of losses or a near miss—such as two out of three cherries on a slot machine—signals an imminent win.
Unfortunately, researchers estimate that more than 80 percent of gambling addicts never seek treatment in the first place. And of those who do, up to 75 percent return to the gaming halls, making prevention all the more important. Around the U.S.—particularly in California—casinos are taking gambling addiction seriously. Marc Lefkowitz of the California Council on Problem Gambling regularly trains casino managers and employees to keep an eye out for worrisome trends, such as customers who spend increasing amounts of time and money gambling. He urges casinos to give gamblers the option to voluntarily ban themselves and to prominently display brochures about Gamblers Anonymous and other treatment options near ATM machines and pay phones. A gambling addict may be a huge source of revenue for a casino at first, but many end up owing massive debts they cannot pay.
Psychology Behind Problem Gambling Addiction
Psychology Behind Problem Gambling Winnings
Shirley, now 60, currently works as a peer counselor in a treatment program for gambling addicts. “I'm not against gambling,” she says. “For most people it's expensive entertainment. But for some people it's a dangerous product. I want people to understand that you really can get addicted. I'd like to see every casino out there take responsibility.”